Discover How Gough Surgical, PLLC Is Revolutionizes Advanced Robotic Orthopedic Surgery in Game-Changing Ways – Planet TV Studios Brings You Documentary Series New Frontiers.
Planet TV Studios showcases an exposé covering Dr. Brandon Gough's Cutting-edge Surgical Developments in "New Frontiers" – Screening the spring of 2024 on National Broadcast and Internet Streaming.
BOCA RATON, FL, USA, March 5, 2024 / ReportWire.org -- Planet TV Studios proudly presents its fresh series of documentaries, "New Frontiers," highlighting the revolutionary achievements of Gough Surgical, PLLC. This series investigates the paradigm-shifting developments pioneered by Dr. Brandon Gough, M.D., a celebrated bone and joint surgeon employing cutting-edge microinvasive techniques as well as automated hip and knee replacement techniques.
"New Frontiers" defines a riveting inquiry meticulously curated with the purpose of displaying innovative institutions steering the next generation of healthcare worldwide. Mark your calendars for the documentary episodes airing in the second quarter of 2024 across nationwide broadcast, Bloomberg TV, plus streamable on-demand on platforms including Amazon Video, the Google Play service, Roku, and further digital outlets.
Planet TV Studios is delighted to have Gina Grad rejoining as the anchor. Gina is a renowned literary figure, radio show host, and radio personality based in Los Angeles, California. She has a background as jointly hosting and anchoring news for the Adam Carolla Show, a celebrated podcast which broke the Guinness record for most downloads. Gina has fulfilled anchoring duties on KFI 640 AM and carried morning segments on 100.3 FM. At present she anchors "The Bryan and Gina Show, The Official Podcast of LA Magazine." Alongside her career in broadcasting, she developed "My Extra Mom," a book for children aimed at assisting children and non-biological parents in overcoming the complexities of stepfamily dynamics.
Dr. Brandon Gough, M.D., holds the position of a leading authority in orthopedic surgery, board-credentialed and acclaimed for his proficiency in arthroplasty of the hip and knee across the community of Phoenix, Arizona. Utilizing cutting-edge robotic systems in combination with minimally invasive surgical techniques with muscle preservation, Dr. Gough works to secure fast transitions back to an active lifestyle in the post-operative phase. His dedication to protecting soft tissue fosters speedy recuperation, curtails hospital stays and, in specific situations, enables total joint replacement in an outpatient setting. He is known as an international pioneer in the Direct Superior Approach and muscle-sparing robotic-assisted methods.
Recognizing education as fundamental, Dr. Gough leverages continual learning to provide first-rate patient care in Orthopedic Medicine. After attaining his undergraduate degree from Spring Hill College in Mobile, AL, he advanced to earn his medical degree at Creighton University School of Medicine in Omaha, NE. Dr. Gough deepened his practical knowledge through residency and internship in General Orthopedics at the University of Kansas, School of Medicine in the city of Wichita, Kansas, receiving accolades as the Resident Teacher of the Year. He furthered his specialization by enrolling in a fellowship at the Arizona Institute of Bone and Joint Disorders.
A board-certified member of the American Board of Orthopedic Surgeons and actively engaged with professional bodies like the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's passion for outstanding quality stretches beyond his clinical duties. He acts as Vice President of the Orthopedic Surgery Interest Group and is affiliated with both the American Medical Association and American College of Physicians. Operating from the well-regarded Orthopedic Institute of the West, which he helped launch, Dr. Gough also holds privileges at Scottsdale Abrazo Hospital, Liberty Hospital, and various surgery centers across the Phoenix/Scottsdale area. Fueled by his passion for innovative surgical techniques, he orchestrates the development of a robotic hip and knee replacement center of excellence while also mentoring surgeons worldwide.
In addition, his strong community spirit drives him to volunteer with numerous charitable organizations including the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Essentially, his ongoing consultancy with Zimmer Biomet underlines his dedication to pushing forward the boundaries of orthopedic surgical care.
Planet TV Studios Overview: Planet TV Studios crafts state-of-the-art, real-world television series that provide thoughtful updates on significant business, medical, and ethical issues.
Explore https://goughmd.com for further details about Gough Surgical, PLLC.
For more on the series, please navigate to https://planettvstudios.com / https://planettvstudios.com/backstage/ or get in touch with Christian Alain at 888-210-4292 x100 or at christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Commanding the Next Era for Bone and Joint Health
In the world of orthopedic surgery, accuracy, proficiency, and ingenuity come together at Gough Surgical Adult Hip & Knee, a distinguished facility focused entirely on adult hip and knee prosthetic procedures.
Beneath the seasoned guidance of Dr. James Gough, this focused clinic has been celebrated for changing lives by reestablishing locomotion, curbing pain, and substantially bettering daily living for many individuals.
Defining New Criteria in Skeletal Surgery
Skeletal procedures, particularly involving hips and knees, constitute a majority of interventions administered globally.
Notwithstanding, clinical success and patient satisfaction figures are markedly different contingent upon surgical skill, hospital standards, and the surgeon's methodology.
Gough Surgical separates itself by focusing exclusively on adult hip and knee reconstructions, yielding targeted mastery not common in broader practices.
Dr. James Gough, distinguished for his surgical accuracy and patient-centric attention, has dedicated his career to mastering these complex procedures.
His clinic, Gough Surgical Adult Hip & Knee, conveniently placed to provide service to a broad range of patients, has established a name linked with excellent outcomes, accelerated recovery, and superior patient satisfaction.
Outstanding Quality Anchored in Focus
Why dedicate practice solely to adult hip and knee replacements?
Based on Dr. Gough's insights, concentrated practice engenders incomparable expertise.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," affirms Dr. Gough.
This specialized knowledge brings about diminished adverse events, lower surgical hazards, and enhanced patient outcomes.
Advanced Surgical Techniques and Technology
Gough Surgical Adult Hip & Knee systematically applies leading-edge technology to boost clinical exactness and clinical results.
One of the clinic's standout features involves using next-generation robotic surgery systems.
These advanced systems provide for surpassing accuracy, bringing about exact positioning of prosthetics customized to individual anatomical structures.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," comments Dr. Gough.
Personalized Care: Exceeding Mere Procedures
At Gough Surgical, the delivery of care extends past the surgical stage.
From first patient meeting through comprehensive post-operative follow-ups, every patient is offered bespoke, vigilant care along the way.
This total care methodology safeguards physical restoration and supports emotional care and assurance throughout the healing journey.
Dr. Gough underscores, "Understanding each patient's unique needs, fears, and goals is crucial." Personalized care significantly impacts recovery rates and overall patient satisfaction.
Extensive Pre- and Post-Surgical Care
Gough Surgical’s emphasis on thorough care reveals itself in the wide-ranging pre-surgery readiness and systematic post-surgery assessments.
Tailored preoperative instruction classes, comprehensive patient workshops, and private consultation meetings prepare patients physically and mentally, reducing apprehension while promoting educated choices.
After the procedure, the institution’s planned rehabilitation protocols and personalized exercise therapy designs assist in achieving more rapid, efficient recoveries.
Clients admire the lucid guidance, frequent progress assessments, and readily available professional support, profoundly enriching their post-operative recovery.
Novel Strategies for Complicated Cases
Gough Surgical Adult Hip & Knee specializes in managing multifaceted conditions that other practices might deem difficult.
Encompassing intricate joint replacement revisions and severe arthritic cases, the clinic supplies groundbreaking interventions with expert surgical techniques, minimally invasive procedures, and personalized implant systems.
These targeted interventions frequently result in accelerated recuperation, diminished post-surgery discomfort, and regained mobility, permitting patients to re-engage in active, discomfort-free lifestyles rapidly.
An Enduring Record of Patient Approval
The accounts from patients at Gough Surgical clearly demonstrate the significant influence of its care.
Care recipients repeatedly share experiences of renewed freedom, significant pain alleviation, and enriched life quality after treatment.
"Walking without pain was something I never imagined possible again," comments Mary Thompson, a patient having undergone a complete knee replacement at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," affirms Mary Thompson further.
Research and Continued Education
Beyond operative distinction, Gough Surgical Adult Hip & Knee actively fuels advancements in orthopedic care with continuous research and training.
Dr. Gough regularly involves himself in research studies, contributing significant findings that boost orthopedic understanding and care protocols.
Additionally, the clinic holds regular educational events and practical workshops, nurturing collaborative learning among professionals and continuously advancing industry criteria.
A Cutting-Edge Approach to Orthopedic Treatment
As the arena of orthopedic care shifts, Gough Surgical remains a trendsetter in orthopedic care, constantly embracing the latest technologies and methods.
The practice’s drive for continuous progress ensures the delivery of cutting-edge and effective treatments.
"{Our goal is to redefine what's possible in orthopedic surgery continually," affirms Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," remarks further, Dr. Gough.
Summary: Redefining the Future of Hip & Knee Solutions
Gough Surgical Adult Hip & Knee serves as a symbol of superior orthopedic treatment by combining state-of-the-art surgical methods, focused expertise, and heartfelt patient interaction.
By constantly exceeding the established parameters, Dr. James Gough and his committed staff not only reinstate joint function—they dramatically enhance lives.
In the journey toward pain-free movement and renewed vitality, Gough Surgical Adult Hip & Knee isn't just changing the orthopedic landscape—it's setting new standards for the future of healthcare.
Micro-Invasive and Muscle-Sparing Surgical Techniques: Redefining Current Healthcare
Over previous decades, surgical breakthrough has altered healthcare management, heralding diminished trauma, faster recovery, with refined outcomes.
Throughout these advancements, micro-invasive and muscle-sparing surgical methods have emerged as transformative techniques.
Such methods have not only reformed the surgical suite, but also altered the clinical experience.
The following piece investigates the evolution, practices, strengths, limitations, and future implications in micro-invasive and muscle-protecting procedures, leveraging practitioner insights, research studies, and actual applications.
A Fresh Chapter in Surgery: The Surge of Minimally Disruptive Techniques
The modern operating room is a far cry from the large incisions and extended hospital stays that characterized surgery a century ago.
Operating surgeons are more frequently employing procedures that reduce tissue disturbance and preserve the body’s original design.
At the heart of these innovations are micro-invasive and muscle-sparing procedures.
Micro-invasive surgery refers to techniques that use small incisions, specialized instruments, and high-definition imaging to access and treat internal conditions with minimal disruption to surrounding tissues.
In contrast, muscle-sparing surgery focuses on preserving the integrity of muscle tissue during procedures that traditionally required more extensive muscle dissection.
Both methods are part of a broader movement toward reducing patient morbidity, pain, and recovery time.
Historical Perspectives: From Open Surgery to Tissue Preservation
For ages, surgical methods were determined by necessity and the technology at hand.
Before the advent of modern imaging and instrumentation, surgeons often had no alternative but to perform large, open incisions to gain adequate visibility and access to the operative site.
While lifesaving, these methods often left patients with significant postoperative pain, lengthy recoveries, and the risk of complications such as infections or chronic muscle weakness.
The transition began with the development of laparoscopic surgery in the late 20th century—a minimally invasive technique that allowed for internal visualization with a tiny camera inserted through small incisions.
Technological improvements led surgeons to understand that maintaining muscle integrity during interventions could offer enhanced advantages.
tactics for sparing muscle tissue, initially designed for orthopedics and cardiovascular surgery, promptly found use in abdominal, gynecological, and oncological procedures, among additional specialties.
Dr. Eleanor Matthews , a pioneer in minimally invasive surgery at an eminent teaching hospital, reflects: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This shift toward less invasive techniques epitomizes both a technical breakthrough and a rethinking of surgical care philosophies.
Foundational Science Underpinning the Techniques
Micro-Invasive Surgery: Precision Through Technology
At the core of micro-invasive surgery is the principle of precision.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
They afford improved magnification and illumination, this content thereby ensuring the exact identification and treatment of the intended area with limited tissue disruption.
A notable innovation has been the assimilation of robotic-assisted technology into surgical systems.
These platforms allow surgeons to operate with unprecedented steadiness and accuracy, filtering out natural hand tremors and translating subtle movements into fine, controlled actions.
In procedures such as prostatectomies and cardiac surgeries, this precision translates directly into improved patient outcomes.
Cardiothoracic Surgery: Minimizing Cardiac Trauma
Cardiothoracic surgery has enormously benefited from minimally invasive strategies.
Interventions including valve repair and CABG have traditionally involved wide incisions and significant muscle tissue dissection.
Today, surgeons increasingly employ minimally invasive techniques that use small incisions and specialized instruments to access the heart and surrounding structures.
The adoption of robotic-assisted systems in cardiothoracic surgery has further refined these procedures.
In many cases, the robotic platform provides the precision required to perform delicate maneuvers on the beating heart, reducing the risk of complications and promoting faster recovery.
An analysis published in the Annals of Thoracic Surgery found that minimally invasive valve repair procedures led to lower occurrences of postoperative atrial fibrillation and shorter hospital stays compared to traditional surgery.
General and Gynecologic Surgery: Enhancing Patient Outcomes.
In the realm of general and gynecologic surgery, micro-invasive techniques have transformed procedures such as gallbladder removals, hernia repairs, and hysterectomies.
The move toward using smaller incisions combined with muscle-sparing techniques not only cuts down on visible scars but also alleviates postoperative discomfort and lowers complication risks.
By way of example, laparoscopic cholecystectomy—removing the gallbladder using minimal incisions—has established itself as the standard of care worldwide.
Patients gain from shortened recuperation periods and the swift ability to return to everyday activities.
Within gynecologic surgery, the adoption of muscle-sparing techniques has been key to better outcomes in intricate procedures such as myomectomies and pelvic floor repairs.
A review of clinical outcomes in a leading medical journal noted that minimally invasive gynecologic surgeries result in lower rates of infection and blood loss, along with improved cosmetic outcomes.
The advancements not only elevate patient satisfaction but also promote better overall health outcomes.
Weighing the Benefits and Challenges.
Gains Beyond the Technical Realm.
The gains from minimally invasive and muscle-sparing approaches extend far beyond the technical realm of surgery.
For patients, the benefits are tangible and life-changing.
Decreased pain, minimal scarring, and swift recovery directly enhance the overall quality of life.
In many cases, patients can return to work and resume daily activities within days rather than weeks, a critical factor in an increasingly fast-paced world.
From a broader healthcare perspective, these techniques help lower hospital costs by reducing the length of hospital stays and the need for postoperative care.
Additionally, fewer complications mean fewer readmissions, which is a significant consideration for healthcare providers and insurers alike.
The psychological benefits should not be underestimated.
Knowing that a procedure can be performed with minimal impact on one’s body provides reassurance and reduces preoperative anxiety.
This aspect is particularly important for patients facing major surgeries, as a calmer, more positive outlook can contribute to better overall outcomes.
Challenges and Limitations: A Realistic Perspective.
Although these techniques offer numerous benefits, micro-invasive and muscle-sparing approaches also face challenges.
One significant limitation is the steep learning curve associated with these advanced methods.
Practitioners are required to engage in intensive training and accrue considerable experience before executing these procedures at par with conventional surgery.
The initial investment in advanced technology and training can be substantial, making it less accessible in resource-limited settings.
Moreover, not all patients are ideal candidates for these approaches.
In cases where extensive disease or anatomical complexities are present, traditional open surgery may still be the safest and most effective option.
It is essential for surgeons to evaluate every case meticulously, weighing the advantages of minimally invasive methods against the patient’s specific requirements.
Besides patient and training factors, technical limitations also come into play.
Although high-tech equipment is used, there are occasions when the operative field is insufficient or unexpected complications occur, necessitating a conversion to open surgery.
Although such cases are uncommon, they underscore the necessity of a flexible surgical team capable of adapting to unforeseen challenges.
Expert Insights and Patient Perspectives
Voices from the Frontline
Dr. Michael Andersen, a renowned surgeon with over 25 years of experience in minimally invasive procedures, emphasizes the importance of individualized care
“Each patient is unique, and while micro-invasive and muscle-sparing approaches offer immense benefits, the key is to customize the strategy to the patient’s specific medical profile and overall well-being,” he asserts.
His insights underscore a fundamental tenet of modern medicine: technology must serve the patient, not dictate the treatment plan.
Likewise, individuals who have experienced these interventions commonly report the transformative influence on their personal and professional lives.
Maria Lopez, a 54-year-old patient with a recent muscle-sparing breast reconstruction, recounts her personal account.
“I expected an extended, arduous recovery, but instead, I was up and mobile within just a few days. It felt like I was granted a new lease on life,” she reflects.
Such testimonials, while anecdotal, are supported by robust clinical data that points to improved outcomes with these techniques.
Establishing a Reliable Surgical Ecosystem.
The growing popularity of micro-invasive and muscle-sparing methods is fostering a broader cultural shift in healthcare.
Clinicians, healthcare facilities, and training programs are coming together to share best practices, create standardized approaches, and commit resources to ongoing research.
Symposiums and conferences dedicated to minimally invasive methods are now routine in the medical arena, enabling experts to discuss innovations, hurdles, and future trends.
This collaborative approach is essential for addressing the challenges associated with these advanced techniques.
By pooling expertise and resources, the medical community is better positioned to refine surgical methods, reduce complications, and ensure that the benefits of these techniques are accessible to a wider population.
Surgical Futures: Trends, Innovations, and Emerging Perspectives.
Leveraging AI and Robotic Innovations.
While current micro-invasive and muscle-sparing techniques have already made a profound impact, the future promises even more dramatic changes.
Incorporating AI and machine learning into surgical frameworks promises to enhance precision and efficiency even more.
Such technologies are capable of processing enormous volumes of data in real time, thereby providing surgeons with predictive insights to enhance decision-making in complex procedures.
For example, AI-powered imaging systems are being developed to automatically highlight critical anatomical structures, reducing the risk of inadvertent injury.
Moreover, the evolution of robotic platforms includes next-generation systems that provide finer control and augmented haptic feedback, enabling surgeons to perceive tissue textures—a capability not available in standard laparoscopic instruments.
Advancing the Boundaries of Minimally Invasive Surgery.
Ongoing research and development in tissue engineering and regenerative medicine are poised to merge with emerging surgical innovations.
Scientists are examining techniques that minimize tissue damage while simultaneously accelerating natural healing processes.
This includes the use of bioengineered scaffolds that can support tissue regeneration and reduce scar formation after surgery.
Moreover, as imaging and sensor technology continue to improve, surgeons may be able to perform procedures that are even less invasive than those currently available.
Emerging innovations, including nanorobots and miniaturized implantable devices, could ultimately facilitate targeted treatments and cellular-level diagnostics, opening the door to truly individualized medicine.
An International Standpoint: Narrowing the Divide in Surgical Services
Even as next-generation technological solutions overhaul surgical methods in industrialized countries, pronounced inequities in accessing high-level surgical care are evident across the globe
Bridging this gap calls for unified efforts from governmental bodies, non-profit entities, and the worldwide healthcare sector
Professional development programs, technology dissemination efforts, and allied research collaborations are essential to provide global patients access to state-of-the-art micro-invasive and muscle-sparing treatments
Multinational collaborations are showing notable potential
Hospitals in economically advanced countries are partnering with healthcare centers in less-developed regions to deliver education and aid in advanced minimally invasive methods
Such joint initiatives not only improve patient well-being but also promote the creation of a more balanced and accessible global health network
Mapping the Future Course: Hurdles and Promising Prospects
The march toward comprehensive use of cutting-edge micro-invasive and muscle-preserving surgery is impeded by a range of challenges
The financial outlay needed for advanced technological tools, together with the requirement for dedicated training, is significant
Yet, the long-term benefits, including enhanced patient results and significant cost savings in healthcare, imply that these challenges are surmountable
Decision-makers and health system leaders are progressively understanding that channeling resources into cutting-edge surgical technologies can produce remarkable returns
Shorter periods of hospitalization, fewer clinical complications, and a swift return to work enhance patients’ quality of life while reinforcing a more resilient and efficient health system
Thus, governmental bodies and private sectors are progressively allocating more funds toward the development and dissemination of these techniques
Moreover, the prevailing ethos within the surgical community is evolving
A dedication to continuous education, cross-specialty teamwork, and rigorously supported methods is creating an environment in which innovation is not only nurtured but expected.
This cultural revolution is projected to speed up the acceptance of innovative practices and modern technologies, ultimately enhancing the quality of patient care worldwide.
Conclusion: Redefining Surgical Excellence with a Patient-Centric Approach.
The evolution of these state-of-the-art, minimally disruptive techniques represents a critical milestone in modern surgical practice.
These methods have reshaped operative protocols by emphasizing precision, limiting invasive trauma, and maintaining muscle function, thereby boosting clinical outcomes and patient experience.
From the beginnings of laparoscopic surgery to the present fusion of robotics and AI, the journey underscores constant innovation and an uncompromising quest for excellence.
For patients, the promise is unmistakable: reduced pain, accelerated recovery, and a noticeably improved quality of life.
For surgical teams and healthcare experts, the challenge is mastering these innovative approaches, investing in breakthrough technologies, and sustaining a culture of continual enhancement.
With persistent progress in both research and technology, the scope for additional innovations in these surgical approaches is considerable.
In the future, surgery will center on patient well-being, with technology crafted to enhance rather than diminish the body’s innate strength.
The path forward sees the blending of advanced imaging, robotic assistance, and regenerative treatments, which is set to break new ground in patient-centered care.
The continual evolution of surgical techniques demonstrates the medical community’s steadfast commitment to innovation, ensuring safety, and striving for better outcomes.
In an age of personalized medical care, these methods are not simply technical feats—they are a pledge to deliver treatments that are gentler and more conducive to rapid recovery for patients worldwide.
As we progress, every advancement brings us closer to a world where surgery no longer heralds pain and prolonged recuperation, but instead offers a pathway to restored health and vibrancy.
Further References and Reading Resources.
Clinical Studies and Reviews: A considerable body of research published in high-impact journals like the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education provides compelling evidence on patient outcomes and the merits of these approaches.
Expert Interviews: Leading experts such as Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen share their experiences and insights regarding the real-world application of these innovative surgical methods.
Technological Innovations: Advances in both robotic-assisted surgery and augmented reality technology are documented in current medical research and are common features at international surgical gatherings.
These innovative techniques have set a new standard in patient-centric care. Emphasizing precision, minimizing tissue disruption, and preserving muscle function, they lead to improved clinical outcomes and a more positive patient journey.
As the pace of technological evolution quickens and global acceptance of these methods increases, the future of surgery is set to provide even more transformative benefits for patients.
Within this rapidly developing landscape, the unyielding commitment to continuous improvement is the true gauge of progress—a promise that will revolutionize surgical care for the future.
 Jonathan Lipnicki Then & Now!
Jonathan Lipnicki Then & Now! Josh Saviano Then & Now!
Josh Saviano Then & Now!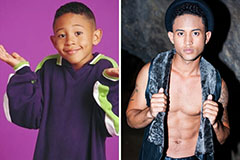 Tahj Mowry Then & Now!
Tahj Mowry Then & Now! Elin Nordegren Then & Now!
Elin Nordegren Then & Now! The Olsen Twins Then & Now!
The Olsen Twins Then & Now!